Emergency Medicine
I am sure that you will have an excellent attachment with us and we look forward to your joining us.
The Emergency Department is a busy place and it is normal to feel a little apprehensive prior to starting, particularly if you haven’t spent much time in the ED previously.
Please be reassured that you will never be on your own, and you will be fully supported. There is a speciality doctor on duty with you 24hrs, along with a consultant until midnight every day of the week.
I would also recommend using the resources of our experienced nurses, both in majors and particularly in minors. We fully understand that for most of you this will be your first time dealing with minor injuries. It is quite normal, and expected, for you to discuss the x-rays you have taken. We fully appreciate that at first it can be very daunting to see and discharge patients.
I am sure that the “4hr target” won’t have passed you by. One misunderstanding can be that the 4hr target refers to the waiting time to be seen. It is worth clarifying at this early stage that this is not the case – the patient must have left the department within 4hrs – either being discharged home or admitted to a ward.
The overall management of the flow through the department is predominately the responsibility of the Consultants, Senior Nurses and speciality Doctors. However it is expected that you be aware of how long your patients have been in the department and seek advice or make decisions early.
It is vitally important that decision inertia doesn’t set in. For the vast majority of ED patients it will be clear after taking the history and examination whether this patient will be coming in or going home – communicate this to the nurses in minors or the medical team leader (wearing a red badge!) in majors prior to sitting down to write your notes. Fundamentally – ask questions, we expect you to discuss every patient to begin with – all we ask is that you make a provisional plan, please don’t sit on patients waiting for all the tests to come in prior to discussing a case.
Finally – remember why you first chose a medical career. Think about the patients and their relatives. A little reassurance or the offer of a cup of tea can go a very long way. Introduce yourself as Dr xxxx, try and avoid first names – both yours and patients’.
Patients will get tired and irritable, understand this and empathise with them, be your patient’s advocate.
Working in the emergency department is incredibly rewarding, don’t let concerns over the 4hr target distract you from the real privilege of working with a team of motivated clinicians helping 200-250 patients a day who have come to us because they have nowhere else to turn!
Welcome to the team!
Nick Laundy
ED Consultant and Clinical Lead
COVID19
These pages have been updated to reflect the adaptations we have made to manage patients presenting with possible COVID19. This clearly remains a rapidly evolving area – please follow this link to our latest COVID19 SOP.
The Department
The Emergency Department (previously known as the Accident and Emergency Unit) serves both urban and rural areas over a large geographic catchment area. This includes Cheshire, the Wirral and parts of North Wales.
We have approximately 85,000 annual attendances to the department. 15,000 of these are seen by our Primary Care Unit (PCU) which is GP and Advanced Nurse Practitioner (ANP) led, whilst the remainder are seen within the ED.
Medical Team
The Consultant / senior medical team is made up of:
- Mr Laundy – Clinical lead
- Dr Wilson – PCU/Major Incident/Simulation/Resus lead, Trust Trauma Lead
- Dr Thevendra – Ultrasound/SHO teaching/Simulation/Resus lead
- Dr Tinker – Sepsis lead
- Mr Mittal – Antibiotic/Oncology/RCEM College Tutor
- Dr Davison – Minor Injuries Lead, Recruitment Co-ordinator
- Dr Holder – Audit lead
- Dr O’Brien (locum) – Rota lead
- Dr Zafiru – Associate Specialist
There are 3-5 Specialist Trainees in the department and a number of substantive middle grades whom all have significant EM experience.
We are supported by the Advanced Nurse Practitioners (ANPs) who are nurses who have completed further training (including prescribing). They work independently, however they may not see certain cases (such as paediatrics) if they feel it is outwith their training. The ANPs will often support the other nursing staff such as in resus and offer a valuable resource for the department.
Nursing Team
The Nursing team is headed up by Matron Jarvis who is based in the ED. She is responsible for a team of approximately 100 nurses and healthcare support workers. There is always a senior (Band 7) nurse in the department and a supernummary team leader in majors. They are recognised by their navy uniforms. Please listen to them, as many of them have years of experience and have been in place longer than the Consultants!
We have a well-established Emergency Nurse Practitioner (ENP) service who see and manage the majority of minor injuries in conjunction with our department physiotherapists.
There is a Trust Trauma Co-Ordinator (Sister Milliken) who liaises closely with the department on trauma care and will attend trauma calls when available.
We also have 3 nurses who take a nursing lead in all aspects relating to resuscitation (Sisters Welsh/Ralphs and CN Jones). They are involved in development of the physical room, protocols and training.
Physician Associates (PA)
We have a number of PA’s, both locally employed and on secondment from Liverpool heart and chest hospital. PA’s can take a history, examine, cannulate and devise management plans for their patients including admission / discharge decisions. However they currently cannot request ionising radiation investigations or prescribe medication. They may therefore approach you for assistance in these areas, however be cognisant that you are responsible for making a clinical judgement about the appropriateness of all prescriptions and investigations you make.
Specialities on Site
- Medicine
- Acute Medicine
- Cardiology
- Respiratory
- Diabetes and Endocrine
- Care of the Elderly
- Gastroenterology
- Stroke
- Rheumatology (not out of hours)
- Dermatology (not out of hours)
- Anaesthetics
- Intensive Care (Adult)
- Paediatrics inc neonatal
- Obstetrics and Gynaecology
- Surgery
- General (Lower and Upper GI)
- Orthopaedics
- Plastics (no burns service)
- ENT
- Vascular hub (SMART centre)
- Ophthalmology (no in-patient beds)
- Maxillo-Facial (not out of hours)
Layout
The department is split into a number of areas/streams:
- RED zone
- All those with signs/symptoms of COVID19
- Space for 12 trolleys including 3 side rooms in our old Majors area
- Including Resus room for COVID19 possible patients.
- Majors
- e.g. cardiac sounding chest pain
- Patients requiring a trolley / monitoring (no signs/symptoms of COVID19)
- Space for 7 trolleys in our old Ambulance offload area.
- Ambulatory Majors
- Patients not requiring a trolley/monitoring who aren’t suitable for PCU or minors
- Patients remain in main waiting room and are called through to available cubicle
- Resus
- e.g. acutely unwell ?AAA
- non-COVID19 patients.
- Minors
- e.g. minor head injury/twisted ankle
- Patients wait in minor injury unit / PCU waiting room
- Clinical Decision Unit (CDU)
- A comfortable area where suitable patients can wait for the results of investigations.
- Patients must be ambulant or able to sit in a chair and not be requiring monitoring or on-going nursing intervention. (no COVID19 signs/symptoms)
- Primary Care Stream
- e.g. sore throats/non-acute limb problems
- Patients wait in minors/PCU waiting room
- Seen by PCU clinicians working within our Ambulatory Majors area
- Paediatrics
- Patients wait in separate paediatric waiting area
- Separate 3 cubicle paediatric area.
- Children requiring resus facilities are seen in the paediatric bay of Resus
Ambulances bring patients for all streams and those with no symptoms or signs of COVID19 are assessed on arrival in the majors department (some may go direct to the waiting room or minors depending on the presentation and ambulance crew) and then are directed to the most appropriate area.
Those presenting with symptoms or signs of COVID19 are directed to an available trolley space within the RED zone.
The majority of the medical and surgically accepted patients should be seen in the respective assessment units: ACU (Ambulatory Care Unit), GPU (GP Unit), SAU (Surgical Assessment Unit), GAU (Gynae Assessment Unit)
However, when these units close, or when patients require intensive monitoring or resuscitation they will attend the ED.
They are normally identified via the bed bureau and should be assessed on arrival by a middle grade or senior Doctor and the appropriate speciality informed. If a speciality accepted patient is identified, then the speciality should be informed and the Meditech system updated. It is the specialities responsibility to manage and investigate these patients; you are not expected to be acting as phlebotomists or be ordering investigations on their behalf. Obviously, should the patient require active resuscitation then we should be starting this.
Referring patients
If there are any problems with referring patients, please let a senior know. We suggest that you introduce yourself as Dr X from the ED – your grade is irrelevant to the process! Make it clear that it is a referral for admission rather than asking for an opinion. Please remember that if you discharge a patient based off the verbal advice of a speciality Doctor, you are still responsible for that patient.
If there is any doubt about the need to admit, please discuss the case with the medical team leader or senior Doctor. We are aiming to start passing all the referrals through the Medical Team Leader to help improve the process.
Please remember that referral is part of the management plan, not necessarily the end step. There is often no need to wait for blood results and x-rays before referral; again, if there is any doubt please discuss with the medical team leader. However likewise, following referral it is important to review outstanding blood results / imaging and ensure they are acted upon and the update the relevant specialty.
Referral process / bleep numbers
This is currently in flux whilst the trust responds to the challenges of COVID19.
The latest process will be explained during local induction.
Computer System
The Countess of Chester currently uses the Meditech computer system. Please ensure that you update the system when you pick up a patient with your name/code -do this prior to seeing the patient.
Once a decision to admit has been made, please update the status to “Bed requested” for the appropriate speciality and inform the Nurse Team leader who will ensure that a bed request is placed on the TeleTracking system.
All the ED clinician documentation should be completed using PDOC – please ensure that you sign off your notes prior to discharge or transfer. We suggest that you treat these notes like traditional written ones, where you add addendums and change the discharge letter as required.
Students
For over 15 years the Countess of Chester Hospital NHS Foundation Trust Emergency Department (ED) has welcomed groups of final year students from the University of Liverpool as well as elective students from other organisations. The Liverpool students are assessed by portfolio in a similar manner to foundation doctors; electives are dependent upon the requirements of the specific university to which the student belongs. These medical students have now be joined by student physician associates.
We are proud of the quality of education we offer our students, be this acute teaching in majors, minors and resus or classroom sessions supported by the senior medical staff. The students will work alongside you on a full shift programme in order to experience the diversity of emergency presentations.
The feedback we receive from students in the ED is usually very good and a relatively large number of our students return to work in the hospital. The feedback from the most recent University review was excellent and some specific teaching practice was praised.
Students should be treated as a member of the team and afforded this level of respect. However, they are not qualified and any patient they see must be physically reviewed prior to any investigations, treatments or discharge. The students should be encouraged to document on the ED notes, including a diagnosis and management plan, and to date, time and sign these appropriately. At present, they do have access to view results on the computer system, but not to document and order investigations.
Teaching
F1/F2/Core Trainee teaching:
- Every Friday morning from 8-9am in the ED seminar room in minor injuries.
- The teaching programme is displayed on the junior doctors notice board.
- Doctors finishing nights and those starting at 8 & 9am are required to attend. Attendance for doctors on other shifts is voluntary
- There is compulsory FY teaching (Wednesday for FY2, Thursday for FY1). Foundation Doctors will be released from daytime duties in the ED to attend these. Unfortunately, we cannot release from nights to allow attendance.
- ACCS and GP VTS will need to apply for study leave (as per the leave section) to attend their regional teaching.
Speciality Doctors/Trainee teaching:
- Trainees are currently scheduled to attend regional teaching on the Tuesday afternoon – the site of this rotates and is co-ordinated by the WhatsApp group.
- We are endeavouring to start regular teaching sessions for all middle grades on Friday mornings; if you have any specific requests please contact Mr Mittal.
Safeguarding
All staff working in the ED have a responsibility to be aware of the potential for safeguarding issues to arise, be it in the context of injured children, young people being vulnerable owing to domestic violence in the home, poor parenting issues or with vulnerable adults attending with illness or injury. The Department supports this through induction training and supporting the release of staff to attend Trust sponsored training. This is available as face to face sessions or on-line training modules.
All ED clinical staff are required to undergo Level 2 and Level 3 training in safeguarding children – the latter also has a section on Domestic Violence as well as highlighting the international problem of Female Genital Mutilation. The Department also has other resources to support staff. All recent bulletins appertaining to SG are displayed on a specific noticeboard on the ED corridor near the coffee room. There you will also find the names of specific staff who specialise in SG matters – from both the ED and Child Health.
The key action you must take when faced with a safeguarding dilemma is to escalate the case through discussion with other colleagues. Level 3 training will help you understand the actions that may follow when such action is taken.
Audit and Research
The department has an active audit program and participates in the RCEM audit system in addition to the internal ones. The program has been very successful over the years leading to a number of changes within both the department and trust and people have had the opportunity to display their work at national conferences.
If people would like to participate in audit, then could they please discuss this with Dr Holder. There are on-going departmental audits which you can partake in or if you have something specific that you would like to look at, please let us know.
The trust has a significant research interest which does include the ED. We have been participants in the CRASH series of trials and PARAMEDIC 2. If you have a specific interest, please speak with Dr Holder.
Targets
As you may be aware (especially from the national press) there is a 4 hour target for patients in the ED; this is NOT an ED-only target, but something that reflects upon the whole trust and requires the entire system to function in order to achieve.
Currently, the target is that 95% of patients should have left the department within 4 hours from their booking in time. Deposition of the patients may include discharge, admission to CDU or admission to a specialty ward. Whilst you need to be aware of this target, you should not let it compromise your clinical care.
Due to the target, the MTL will often be asking you about your patient – as before, please note that referral should be part of your plan not the end-point; do not wait for investigations that will not change your patient’s management (e.g. bloods in a patient with appendicitis). If there is any resistance to this from the specialties, please let a senior know. There have been instances where the specialties do not appreciate the pressure in the ED (from both targets and the elasticity in accommodating patients), equally we are not aware of the pressures elsewhere in the trust.
Various conditions have targets (CQINS) attached to them – these are mainly time-critical interventions such as thrombolysis for CVA and neutropenic sepsis. Again, clinical need may precedent other cases over these.
Sepsis
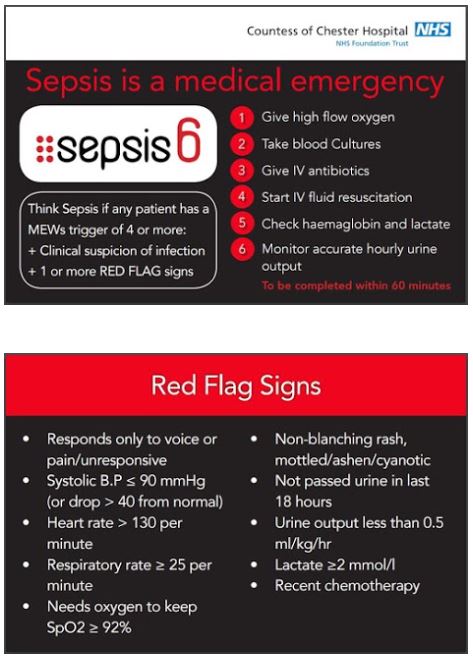
Sepsis is currently very topical in both the national and medical press, understandably so. There have been significant advances over the last 10 years in the management of sepsis. To this end, the trust has its sepsis6 campaign which is promoted around the buildings. Please consider sepsis and early antibiotics in your patients!
Paediatrics
The department enjoys a healthy relationship with children’s services but you must remember that their department is some way from the ED – “over the bridge” – which can lead to problems in safe transfer of patients or the availability of their staff to come to the ED. Hence the need for careful consideration of when a child is fit to be transferred. When in doubt seek senior medical advice. A Paediatric Advance Nurse Practitioner (APNP) is often available during normal hours to provide assistance when a referral may be borderline or the medical team are simply too busy to come over (bleep 3459).
Crash calls to Paeds for collapsed children almost invariably receive a brisk response from their team. Do take some time to check out the Paediatric resuscitation facilities in Resus to better support them when they arrive.
At certain times of day, children are brought to the ED with relatively minor complaints - don’t forget that the Department operates a primary care “stream” that may be able to take this child from you, once a brief clinical assessment has been made.
When the paediatric ward is closed, they operate a treat and transfer policy where they will direct (and notify the MTL) GP referrals to the ED for them (i.e. paediatric team) to assess. If they require transfer for admission, then the paediatric team should arrange this.
Despite the focus on waiting times and a desire to see patients in “time order,” don’t be afraid to expedite the care of children. They can deteriorate very quickly. Also, they can get distressed, even with mild illness, and getting them home or on to the ward quickly can be to the benefit of everyone!
CVA
The majority of the strokes and TIAs present to the ED and can self present, be brought in by ambulance or be referred in from the community. The last group will normally have been discussed with the stroke co-ordinator prior. The stroke co-ordinator is available 0800-2200 daily and will normally attend and assess any strokes that attend with a view to thrombolysis, investigation and admission/discharge. They will also arrange follow-up in TIA clinic if required.
If a CVA fulfils the criteria for thrombolysis, the pathway should be following.
- During the week days the stroke Consultant will normally attend and administer the thrombolytics.
- Out of hours, but within stroke co-ordinator hours, the stroke co-ordinator will (having assessed the patient) contact the on-call Stroke Consultant who will decide regarding treatment. You may be asked to prescribe and administer the drugs.
- Out of stroke co-ordinator hours – at this point, we have to take a lead! The patient should be assessed and rapidly identified as a potential stroke thrombolysis candidate. There is a telemedicine cart available which should be set up and the on-call Stroke Consultant called. They will then be able to guide you through the NIHSS assessment (if you need the help) and will then make a thrombolysis decision and guide you through the appropriate management.
TIAs should be risk stratified as per the pathway. There is daily high-risk TIA clinics available.
The target is to get any stroke patient requiring admission to the stroke unit in less than 3 hours.
Trauma
We are an accredited trauma unit (TU) as part of the Cheshire and Merseyside Trauma Network. Our major trauma centre (MTC) is based at Aintree Hospital.
Our ED has the unique position of being on the NWAS and Welsh Ambulance Service borders. This means that major trauma in England may bypass the Countess, but Welsh major trauma may still arrive. Hence, you may see what feels like a disproportionate amount of trauma for a TU.
There is a list of triggers to activating the trauma team which is kept above the stand-by phone in majors. Our Nursing staff are empowered to activate the team if they feel it is appropriate. All trauma teams should be lead by a middle grade or above. There is an EM Consultant on-call at all times; please call us if there is any doubt as to whether we are required to attend (currently we don’t automatically attend every trauma call overnight, but will if requested).
Patients should be managed according to the (C) ABCDE principles. The trust runs ATLS course twice yearly and a number of the Consultant staff are Instructors on various national trauma courses (e.g. ETC/ATACC).
We have a trauma nurse co-ordinator (Sr Jackie Milliken) who will attend trauma calls when she is available. She also audits the targets including time to CT scan (ideally less than 60 minutes from arrival) and is involved in trauma education. Sr Milliken also helps on any trauma-related audits.
The final word
If in doubt, ask – don’t be afraid, ask a friend!
Contributions and acknowledgements
Dr David Wilson
Mr Nick Laundy